Acute Management of Behavior Changes in Hospitalized Patients with Dementia - #63
Take QuizIdentify the specific difficult behavior and apply best practice management strategies.
Non-pharmacologic Approach:
-
Identify the specific difficult behavior
-
Mood disturbances
-
Depression in Alzheimer’s dementia commonly manifests as irritability and social isolation or withdrawal.
-
-
Manic-like behaviors
-
Pressured speech, disinhibition, elevated or irritable mood, intrusiveness, hyperactivity, impulsivity, and reduced sleep.
-
-
Delusions and Hallucinations
-
Insomnia (see GFFs #38 & #40)
-
Inappropriate Sexual Behavior (see GFF #53)
-
Intermittent Agitation or Aggression
-
-
Best Practice Strategies to Manage Behavior:
-
Interview the family and nursing staff about potential antecedent events.
-
Perform a comprehensive physical exam.
-
Check vital signs and blood glucose levels.
-
Check skin for vulnerable areas (pressure sore sites, genitourinary/sacral areas).
-
Look for possible fractures or unexplained bruising.
-
Screen for depression using the PHQ2 Scale or the Geriatric Depression Scale (GDS).
-
Screen for delirium using the Confusion Assessment Method (CAM).
-
Consider performing a rectal exam to assess for fecal impaction.
-
-
Obtain labs and imaging as appropriate: consider UA, CBC, BMP, LFTs, CXR and perhaps a CT of the head.
-
Assess for pain, elevated post void residual volume of urine, date of last bowel movement.
-
Critically review the medication list: assess for high risk medications (those with anticholinergic properties), new medications, potential adverse drug events, duplicate medications, recently stopped medications, drug-drug interactions, and dosage for renal function.
-
Provide the patient with their glasses, hearing aids, and/or dentures if available.
-
Assess environment.Determine if the patient had a recent room change or living situation move.Consider if there is a noisy environment or clutter.Assess any IV sites, catheters, sequential compression devices (SCDs), and other lines or devices that could be irritating to patient.
-
Communicate with the patient using clear directions and avoiding medical jargon.
-
Communicate with family and RN staff and nursing facility regarding baseline cognition; assess for current or prior treatment for dementia; review patient chart for past history of possible cognitive impairment, psychiatric history or psychiatric medication use.
-
Educate and support the family and caregivers about agitation, delirium and dementia.
-
Avoid physical restraints in patients with behavior and psychological symptoms of dementia (BPSD)/ delirium unless absolutely necessary for safety and medical care.
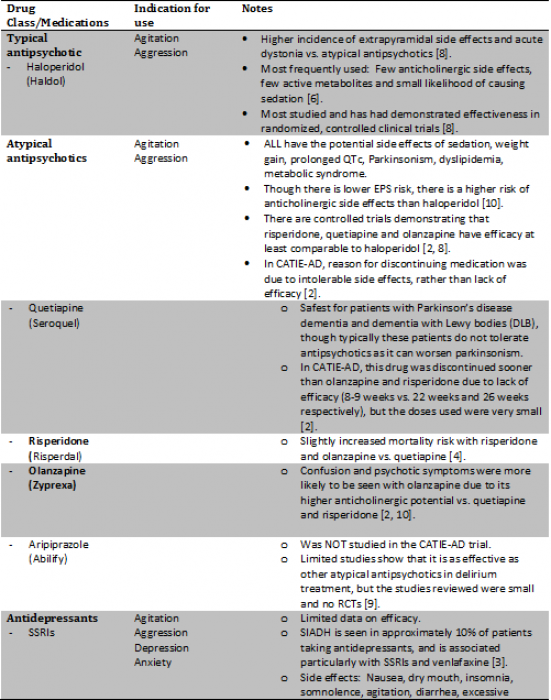
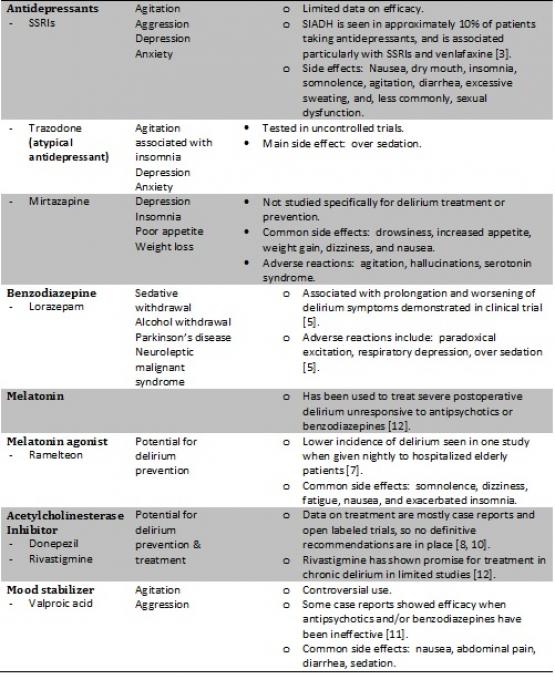
Pharmacologic Interventions
-
-
General ” Best Practice” Prescribing Points:
-
Decrease doses or discontinue any medications which may be contributing to agitation. Review all medications to identify any anticholinergic medications or medications on the Beers’ Criteria:Potentially Inappropriate Medications for the Elderly List.
-
Is the patient in alcohol withdrawal? Consider thiamine and low dose lorazepam if indicated; avoid haloperidol and diazepam.
-
Is the patient exhibiting pain behaviors?Consider scheduled acetaminophen and assess the underlying cause of pain.
-
Are there indications for antipsychotic use? This includes dangerous behaviors to the patient or others; do not use antipsychotic medications for issues of wandering, calling out/yelling, anxiety or sleep disturbance or for inadequate staffing.
-
How do you monitor safe use of antipsychotic medications? Adverse events include increased agitation/paradoxical effect, urinary retention, excessive sedation, swallowing dysfunction (dystonic reaction), QT prolongation.Avoid haloperidol in Parkinson’s disease as it may worsen disease symptoms (quetiapine is likely safer).
-
-
When considering use of antipsychotic or atypical antipsychotic medication, inform family members of the increased risk for increased mortality, pneumonia, CV side effects, increased glucose levels, tardive dyskinesia.Start LOW...one-quarter to one-half the usual starting dose...and increasing SLOWLY if needed.
-
When do you decrease or discontinue antipsychotic medications? The dose of antipsychotic medications should be reviewed daily in the hospital and gradually decreased as symptoms resolve.If the patient needs these medications on discharge, the discharge summary should describe a tapering and discontinuation plan.
-
-
There are NO FDA approved medications for the treatment of agitation in patients with dementia.There is now a black box warning on ALL antipsychotics:conventional and atypical.
-
Approximately 30-40% of cases of delirium are PREVENTABLE.Benzodiazepines and anticholinergic medication should generally not be used as they can precipitate drug induced delirium [8].
Hospitalized patients with dementia who develop agitation or aggression.
- As many as 50%–80% of patients with dementia experience at least one mental or behavioral disturbance during the course of their illness.
- 30% of the cost of caring for patients with Alzheimer’s disease is attributed directly to management of neuropsychological symptoms.
- Prevalence of Specific Behaviors in dementia patients:
- Delusions – approximately 30%
- Hallucinations - up to 20%
- Sleep disturbances – 25-35%
- Sexually inappropriate behavior - 15-25%
Science Principles
Etiologies to Consider:
-
Determine if the behavior is actually due to delirium (consider the Confusion Assessment Methodology Score --CAM score).
-
Define any underlying precipitating factors/antecedent situation.
-
Review medications (medication withdrawal, new or recently stopped medications).
-
Rule out infection.
-
Rule out intoxication (drug, alcohol, other substances).
-
Assess for pain (if present, identify the source).
-
Assess for urinary retention/fecal impaction/skin irritation.
-
Define baseline cognition.
-
Assess/define sensory impairment.
-
Assess (change in) environment, especially overstimulation.
-
Define pre-existing psychiatric comorbidities.
-
Assess for patient frustration with being unable to complete a task that they are asked to perform (i.e. apraxia).
-
Identify any unmet needs (hunger, thirst, incontinence).
- Identify and define agitation in hospitalized patients with dementia.
- Describe non-pharmacologic and pharmacologic strategies for managing agitation.
Review of Systems (ROS)
Geriatric Topics
ACGME Compentencies
Science Principles
-
Pharmacotherapy of Dementia Behaviors Algorithm.Pharmacist’s Letter. October 2011.
-
Schneider L, et al. Effectiveness of Atypical Antipsychotic Drugs in Patients with Alzheimer’s Disease.N Engl J Med 2006;355: 1525-38.
-
Weise B.Geriatric depression: The use of antidepressants in the elderly.BCMJ, Vol. 53, No. 7, September 2011, page(s) 341-347.
-
Maust DT, et al. Antipsychotics, Other Psychotropics, and the Risk of Death in Patients With Dementia:Number Needed to Harm.JAMA Psychiatry. 2015;72(5):438-445.
-
Inouye S, et al. Delirium in Older Persons. N Engl J Med 2006;354:1157-65.
-
Markowitz JD and Narasimhan M. Delirium and Antipsychotics: A Systematic Review of Epidemiology and Somatic Treatment Options. Psychiatry (Edgemont) 2008;5(10):29–36.
-
Perkisas S and Vandewoude M. Ramelteon for Prevention of Delirium in Hospitalized Older Patients. JAMA Psychiatry. 2014;71(4):397-403.
-
Fong TG, et al. Delirium in the Elderly:Diagnosis, Prevention and Treatment. Nat Rev Neurol. 5, 210-220 (2009).
-
Kirino E.Use of aripiprazole for delirium in the elderly: a short review. PSYCHOGERIATRICS 2015; 15: 75–84.
-
Maldonado JR. Delirium in the Acute Care Setting:Characteristics, Diagnosis and Treatment. Crit Care Clin 24 (2008) 657–722.
-
Bourgeois JA, et al. Adjunctive Valproic Acid for Delirium and/or Agitation on a Consultation-Liaison Service: A Report of Six Cases. J Neuropsychiatry Clin Neurosci 2005; 17:232–238.
-
Attard A, et al. Delirium and its Treament. CNS Drugs 2008; 22 (8): 631-644.
Users are free to download and distribute Geriatric Fast Facts for informational, educational and research purposes only. See Term of Use for additional information.
Disclaimer: Geriatric Fast Facts are for informational, educational and research purposes only. Geriatric Fast Facts are not, nor are they intended to be, medical advice. Health care providers should exercise their own independent clinical judgment when diagnosing and treating patients. Some Geriatric Fast Facts cite the use of a product in a dosage, for an indication, or in a manner other than that recommended in the product labeling. Accordingly, the official prescribing information should be consulted before any such product is used.