Performance Improvement in the Nursing Home - #69
Take QuizCreate awareness amongst providers about the role and value in conducting Performance Improvement (PI) programs in the nursing home.
PI in the nursing home (NH) is one of five quality elements designed to improve delivery of care through continuous, proactive and preventative initiatives1. The Centers for Medicare & Medicaid Services (CMS) now requires all NH facilities to develop, implement, and maintain a comprehensive Quality Assurance and Performance Improvement (QAPI) program. Two distinct aspects to QAPI complement each other to make up an integrated quality program: the Quality Assessment (QA) part of the program focuses on meeting quality standards and assuring facility compliance with regulations, and the Performance Improvement (PI) part of the program focuses on process and system improvements to meet the standards of health care delivery and resident quality of life3. PI is the latest synonym for quality improvement (QI).
Create awareness amongst primary care and consultant providers about Performance Improvement (PI) programs and opportunities in the nursing home.
Describe the role and value for conducting PI work in nursing homes.
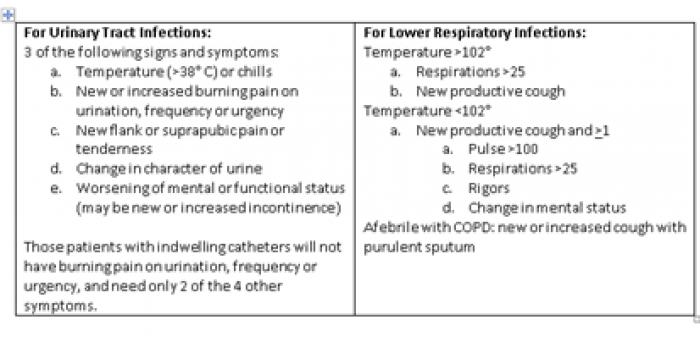
Infection prevention and control: Prevention and management of infection in the NH includes medical management of various infections (e.g., C. difficile, skin and urinary tract infections, multi-drug resistant organisms, flu and norovirus outbreaks) as well as source control and good standard practices such as hand washing and contact precautions. All NHs are now required to have an Antibiotic Stewardship Program to ensure appropriate use of antibiotics, reduce adverse events, prevent antibiotic resistance from overuse, and improve outcomes for nursing home residents7. Different NHs have different infection control protocols that are specific for their population, however, the basic framework for these programs often incorporate the core elements of antibiotic stewardship recommended by the Centers for Disease Control (CDC). This means that on-call, outpatient specialty, and primary care providers need to be aware of their affiliated nursing-home antibiotic stewardship program protocols and communicate effectively with the NH to ensure delivery of safe, appropriate, and quality care to NH residents. One such protocol delineating antibiotic use is the McGeer criteria for UTI and respiratory infections:
Medications: Medication errors8, deprescribing9, and reduction of psychotropic use10,11,12 are among the top PI interventions in the NH. At least 50% of NH patients receive >1 unnecessary or potentially inappropriate medication. Ongoing medication list reviews and deprescribing initiatives focus on individual tailoring of medications for each patient. Placing start and stop dates for medications prescribed by on-call or consulting providers is crucial for optimization of individual medication Reduction of anti-psychotic use initiatives are now focused on non-pharmacologic interventions for management of behaviors and avoiding use of medications associated with high morbidity and mortality.
Transitions of Care and Readmissions: Close attention to transitions between NH, hospital, and community is key. Patients are sicker and more complex, but shorter hospital length of stay means nursing homes accept more complex and medically less stable patients. Hospitals are currently penalized for readmissions within 30 days of discharge and NH will also be included in these penalties starting autumn 2017. Root cause analyses via the INTERACT tool3 are helpful in assisting NHs in identifying preventable readmissions and creating comprehensive care plans.
Other Areas: PI initiatives may also include common problem areas for which process improvements are ongoing: nutrition, skin integrity/pressure injuries, falls, staff training, advance care planning, resident-on-resident aggression, challenging behavior management (e.g., delirium, psychiatric decompensation, dementia10), nursing staff communication, charting, vaccinations, and reporting of change of condition2.
Prioritization of PI initiatives will differ between NHs and is based on the acuity and severity of the problem as well as the magnitude of impact on domains related to resident care (e.g., safety, autonomy, rights, and quality of life). In the nursing home, the focus is to identify opportunities for improvement related to processes and outcomes of care, quality of life, resident choice and facility operations through implementing PI goals and aims (e.g., efficacy, appropriateness, availability, timeliness, effectiveness, continuity, safety, efficiency, respect and caring).
- Identify main areas for PI opportunities in the nursing home.
- Create awareness amongst primary care and consultant providers about PI programs in nursing homes.
ACGME Compentencies
- CMS QAPI Description and Background: https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/QAPI/...
- CMS Resource Guide for Quality Improvement Tools Related to New (April 2016) Nursing Home Compare Quality Measures: https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/QAPI/...
- https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/QAPI/...
- Interventions to Reduce Acute Care Transfers: https://interact2.net/
- Brassard, M., & Ritter, D. (1994). The memory jogger: a desktop guide of tools for continuous improvement and effective planning. New Hampshire: GOAL/QPC.
- Juran, J., & Gryna, F. (1988). Juran’s quality control handbook (4th ed.). New York: McGraw-Hill, 17.4-17.5.
- The Core Elements of Antibiotic Stewardship for Nursing Homes: https://www.cdc.gov/longtermcare/prevention/antibiotic-stewardship.html
- Medication Errors: https://psnet.ahrq.gov/primers/primer/23
- Deprescribing: http://deprescribing.org/
- CMS National Partnership to Improve Dementia Care in Nursing Homes: https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/Surve...
- Cox C, van Jaarsveld H, et al. Psychotropic drug prescription and the risk of falls in nursing home residents. Journal of the American Medical Directors Association. 2016; 17(12):1089-1093.
- Mort J. Antipsychotic medication use in nursing homes: approaches to reduce use and national trends. South Dakota Journal of Medicine. 2015; 68(10):464-5.
- National Nursing Home Quality Improvement Campaign: https://www.nhqualitycampaign.org/default.aspx
- McGeer A, et al. Definitions of Infection for Surveillance in long-term care facilities. Am J Infect Control 19(1):1-7, 1991.