Evaluating Insomnia - #38
Take QuizLearn underlying basic science and practical clinical management of insomnia evaluation.
The following evaluation tools are useful for evaluating sleep disturbances:
- Sleep Questionnaire / History
-
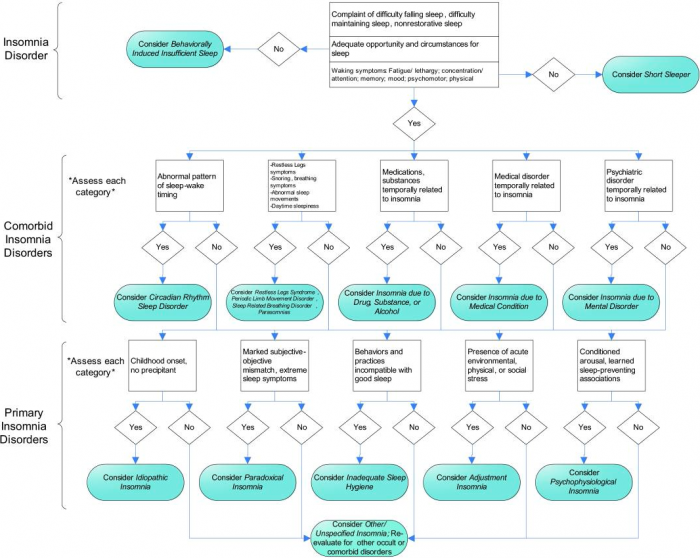
Ask about pre-sleep conditions, sleep-wake patterns, sleep-related symptoms, daytime consequences (see figures 1)
-
- At-home sleep log
- Document for ≥ 2 weeks, continue tracking during treatment
- Psychological screening tests
- Check for comorbid psychiatric conditions (e.g., anxiety, depression).
- Bed partner interviews
- Polysomnography recommended if a breathing or movement disorder is suspected, the diagnosis is uncertain, failed treatment, or violent sleeping habits6
Click on Figure 1 Below to Enlarge
When using this diagram, the clinician should be aware that the presence of one diagnosis does not exclude other diagnoses in the same or another tier, as multiple diagnoses may coexist. Acute Adjustment Insomnia, not a chronic insomnia, is included in the chronic insomnia algorithm in order to highlight that the clinician should be aware that extrinsic stressors may trigger, perpetuate, or exacerbate the chronic insomnia.
Evaluation of sleep disturbances in a geriatric patient
List evaluation strategies for insomnia which may be useful for geriatric patients
Insomnia: Difficulty with sleep which may include: prolonged sleep onset latency, frequent nocturnal awakenings, prolonged periods of wakefulness during the sleep period, or frequent transient arousals .
Geriatric patients commonly experience sleeping disturbances. Although sources differ, up to 60% of geriatric patients report problems with sleeping at least a few nights per week, with 6-15% meeting diagnostic criteria for insomnia(1, 2). Higher rates of insomnia are seen in women, especially after the onset of menopause1. Despite the increased prevalence of insomnia in geriatric patients, insomnia is not normal aging(3). Sleep disturbances in geriatric patients are associated with decreased quality of life, daytime fatigue or low energy, cognitive decline, and mood dysphoria1. The increased prevalence of insomnia in the geriatric population is likely multifactorial in etiology. Comorbid medical, psychiatric, or neurologic illnesses leave patients more susceptible to sleep disturbances, due to the nature of the illness as well as the medications to treat the illness.
Identify strategies for evaluation of insomnia in a geriatric patient.
Review of Systems (ROS)
Geriatric Topics
ACGME Compentencies
- Kierlin L, Olmstead R, Yokomizo M, Nicassio P, Irwin MR. Diagnostic and Statistic Manual criteria for insomnia related impairment in daytime functioning: polysomnographic correlates in older adults. Sleep Medicine. 2012; 13:958-960.
- McCrae CS. Late-life comorbid insomnia: diagnosis and treatment. American Journal of Managed Care. 2009; 15(1):S14-S23.
- Galimi R. Insomnia in the elderly: an update and future challenges. Gerontology. 2010; 58:231-247.
- Morin CM, Benca R. Chronic Insomnia. Lancet. 2012; 379:1129-1141.
- Figure 1 from: Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M. Clinical Guideline for the Evaluation and Management of Chronic Insomnia in Adults. Journal of Clinical Sleep Medicine. 2008; 4(5):487-504.
Users are free to download and distribute Geriatric Fast Facts for Informational, educational, and research purposes only. Citation: Gretchen Wagner, Kathryn Denson, MD, Larry Hook, MD, Elizabeth Nilsson, MD, Dmitriy Shmaryan, MD November, 2013.
Disclaimer: Geriatric Fast Facts are for informational, educational and research purposes only. Geriatric Fast Facts are not, nor are they intended to be, medical advice. Health care providers should exercise their own independent clinical judgment when diagnosing and treating patients. Some Geriatric Fast Facts cite the use of a product in a dosage, for an indication, or in a manner other than that recommended in the product labeling. Accordingly, the official prescribing information should be consulted before any such product is used.
Terms of Use: Geriatric Fast Facts are provided for informational, educational and research purposes only. Use of the material for any other purpose constitutes infringement of the copyright and intellectual property rights owned by the specific authors and/or their affiliated institutions listed on each Fast Fact. By using any of this material, you assume all risks of copyright infringement and related liability. Geriatric Fast Facts may not be reproduced or used for unauthorized purposes without prior written permission, which may be obtained by submitting a written request to: Medical College of Wisconsin, Dept. of Medicine, Division of Geriatrics and Gerontology, 8701 Watertown Plank Road, Milwaukee, WI 53226. Note the Geriatric Fast Facts may contain copyrighted work created under contract with government agencies, foundations, funding organizations and commercial companies, etc. If a particular author places further restrictions on the material, you must honor those restrictions regardless of whether such restrictions are described in this mobile app.