Assessing Dementia Severity - #111
Take QuizAssessment and staging of Dementia determines next care steps for a patient.
Understanding a patient’s placement in the continuum of cognition and cognitive decline is important for increasing patient and caregiver understanding, providing education and appropriate treatment options and advance planning, and optimizing caregiver support.
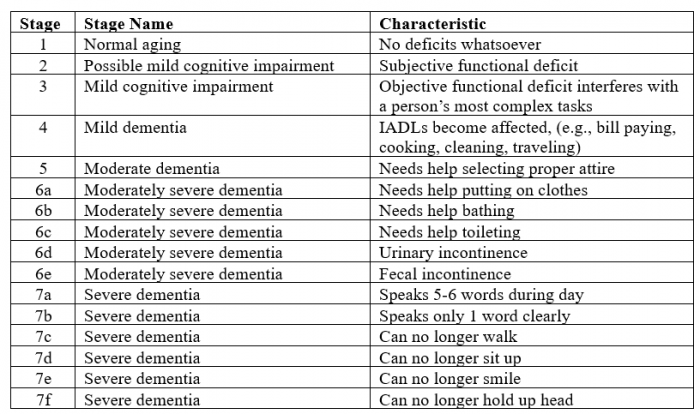
- One of the most utilized tools for the staging of dementia is the FAST (Functional Assessment Staging Tool) Scale, which is best validated for Alzheimer’s dementia:4 (see table) Note: *IADLs: instrumental activities of daily living
- While FAST Staging is generally clear, some additional details and examples may be helpful.
- Staging of dementia3
- A. Stage 1 – no cognitive impairment
- B. Stage 2 – possible mild cognitive impairment
- Examples: subjective cognitive decline reported by patient (memory lapses, forgetting words), without objective evidence of cognitive impairment
- C. Stage 3 – mild cognitive impairment (MCI)
- Some cognitive deficiencies noticeable by friends or family
- Examples: word-finding difficulty, forgetting names, reading a passage and being unable to recall information, misplacing objects, struggles with planning events or activities
- The primary distinction between MCI and dementia is whether function is affected. Patients with MCI may have mild cognitive deficits but are able to compensate without noticeable impairment in functional activities. Patients with early dementia have cognitive deficits which impair function.
- D. Stage 4 –mild dementia (moderate cognitive decline)
- Clear objective deficits in one or more cognitive domains
- Examples: limited knowledge of recent events, forgetting personal history, inability to perform basic math functions, decreased ability to perform complex tasks such as shopping, planning dinner, or paying bills
- Unlike MCI, cognitive decline in dementia becomes significant enough to impair functioning.
- E. Stage 5 –moderate dementia (moderately severe cognitive decline)
- Major gaps in memory and cognitive functioning requiring assistance with daily activities
- Examples: unable to recall their address, phone number, disoriented to time or place, need help selecting proper attire
- F. Stage 6 – moderately severe dementia
- Substantial memory and cognitive impairment, often requiring extensive assistance from others for basic daily activities
- Examples: very little awareness of recent experiences, forgetting loved ones, personality changes, need help selecting proper attire, urine or fecal incontinence, hallucinations, delusions, repetitive behaviors, wandering
- G. Stage 7 – severe dementia
- Patient is unable to meaningfully respond to environment
- Examples: little to no speech, needs assistance with eating or toileting, unable to smile or hold up head, dysphagia, muscle contractures
- 4. Staging of dementia helps inform treatment options:
- A. Monoclonal anti-amyloid therapies are only indicated for patients with mild cognitive impairment (MCI) or mild Alzheimer’s dementia (AD).
- B. Acetylcholinesterase inhibitors may be used for patients with any stage of dementia.5
- C. NMDA receptor antagonists are only approved in patients with moderate to severe Alzheimer’s dementia.5
- D. Rivastigmine is FDA-approved for mild to moderate Parkinson’s dementia.5
- 5. Staging of dementia has prognostic implications:
- A. Patients in later stages of dementia will eventually need full-time care and support (perhaps even palliative or hospice care); it is important to address these concerns and care preferences earlier in the course of disease.
- B. By the time patients have reached FAST Stage 7, they are typically eligible for hospice care (based on their dementia diagnosis) under the Medicare Hospice Benefit, pending other co-morbid states.2
- 6. Staging of dementia has billing/coding implications:
- A. It is important to document:
- type of dementia (e.g., Alzheimer’s, vascular, Lewy Body, Parkinson’s, frontotemporal)
- severity of dementia (e.g., mild, moderate, severe)
- behavioral and psychologic symptoms of dementia (e.g., agitation, mood disorders, psychotic disturbance, anxiety)
- B. “Unspecified dementia” assumes there is no known severity or associated symptoms, and this diagnostic code should generally be avoided.
- C. Precise documentation of the severity of dementia should match the selected charge for the visit and can influence the risk score for reimbursement.
- A. It is important to document:
Determining dementia severity in older adults with cognitive impairment has important prognostic, therapeutic, and billing implications.
Identify and use validated tools to assess dementia severity in patient care.
Globally, an estimated 47 million adults are living with dementia.1
- Describe tools used to assess dementia severity.
- Explain how dementia severity informs management and prognosis.
Review of Systems (ROS)
Geriatric Topics
- World Alzheimer Report 2015: The Global Impact of Dementia http://www.alz.co.uk/research/world-report-2015.
- Medicare hospice eligibility guidelines. https://www.cms.gov/medicare-coverage-database/view/lcd.aspx?lcdid=33393&ver=7&NCAId=96&NCDId=12&ncdver=4&SearchType=Advanced&CoverageSelection=Both&NCSelection=NCA|CAL|NCD|MEDCAC|TA|MCD&ArticleType=Ed|Key|SAD|FAQ&PolicyType=Final&s=5|6|66|67|9|38|63|41|64|65|44&KeyWord=Home+Oxygen&KeyWordLookUp=Doc&KeyWordSearchType=And&kq=true&bc=IAAAABgAAAAA&=
- Harper GM, Lyons WL, Potter JF. Geriatrics review syllabus chapter 41 dementia; page 334-346. American Geriatrics Society. 11th edition; American Geriatrics Society 2022.
- https://www.generationshospicecare.com/2022/06/13/dementia-we-dont-just-forget-end-stage/
- Reuben DB, Kremen S, Maust DT. Dementia Prevention and Treatment: A Narrative Review. JAMA Intern Med. 2024;184(5):563–572. doi:10.1001/jamainternmed.2023.8522